What is erythropoiesis
From the Greek ‘erythro’ meaning red, and ‘poiesis’ meaning to make, erythropoiesis is the complex process that results in mature red blood cells – erythrocytes. This tightly regulated physiological process is one of the most important functions of bone marrow in adults.
There are several types of blood cells, but erythropoiesis specifically refers to the specialized production of red blood cells.
Where does erythropoiesis occur?
Depending on the stage of life, erythrocytes are produced in different areas of the human body.
In the early stages of fetal development, erythropoiesis takes place in the yolk sac, but between two and five months into gestation, this process relocates to the liver and spleen. Finally, at around five to six months, the bone marrow is established as the site of erythropoiesis. Until adulthood, all bone marrow can produce erythrocytes, but upon maturity, production only occurs in the ribs, sternum, pelvis, proximal femur, vertebrae, and sacrum.
What are the stages of erythropoiesis?
From bone marrow to mobilization in the circulatory system, the erythrocyte goes through several complex morphological changes to produce highly specialized cells.
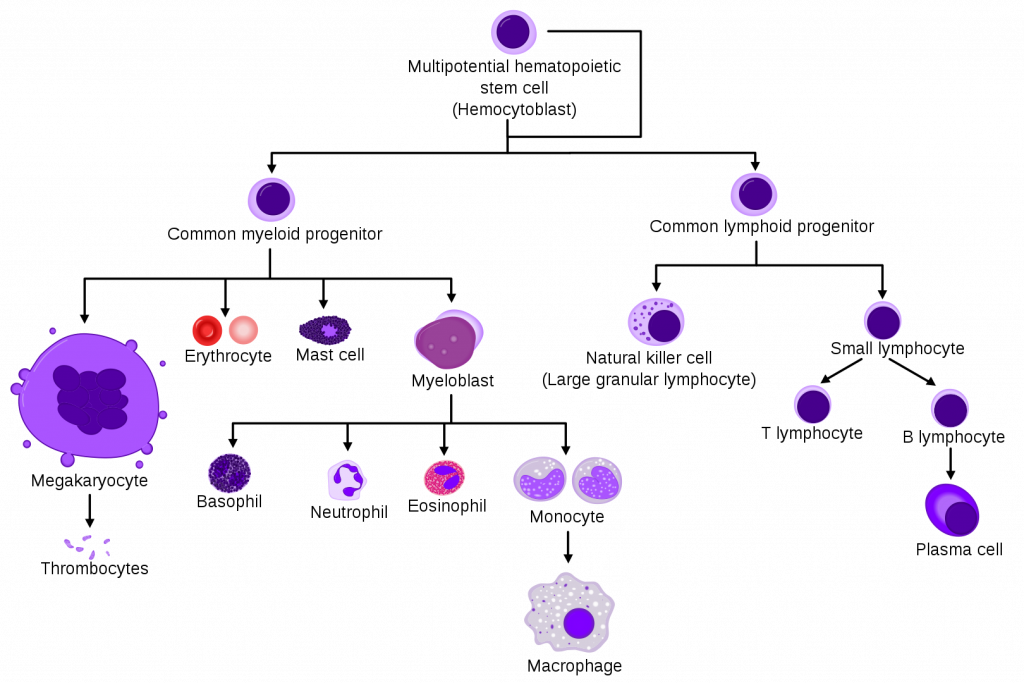
Hemocytoblast
The process begins with the hemocytoblast cells. They develop in the bone marrow and are spongy, loose-formed cells with a large nucleus containing several nucleoli. With the ability to self-replicate, they can be quickly mobilized into the bloodstream when necessary.
As hemocytoblasts are multipotent primordial stem cells, they can start the development process with a number of final goals, including erythroblasts, megakaryocytes, or mast cells. Depending on the body’s tightly regulated cell production, which ensures the necessary number of erythrocytes, for example, are produced, the hemocytoblast becomes either common myeloid progenitor cells or common lymphoid progenitor cells.
The former are the source of the erythrocyte.
Common myeloid progenitor cells
Precursors to a limited number of different cells, including osteoclasts, granulocytes and erythrocytes, myeloid progenitor cells are known as oligopotent. They lack the stem cell’s unlimited ability to self replicate, having a more restricted potency, but still play a major role in ongoing tissue maintenance. Their main function is replacing damaged or dead cells, with the focus on replenishing blood cells.
The common myeloid progenitor cells develop into one of four cell types:
- Megakarocyte Cell – Responsible for the production of thrombocytes, or blood clotting platelets, the megakarocyte cells are large bone marrow cells with lobed nuclei. Approximately 10 – 15 times the size of an erythrocyte, with a diameter of around 50 – 100 μm, they account for 1 in every 10,000 bone marrow cells
- Mast Cell – As part of the immune response system, mast cells help the body fight infections and respond rapidly to certain bacteria, allergens, and parasites. A type of white blood cell, also known as leukocytes, mast cells contain chemicals, including histamine, cytokines, and heparin, which are released when the immune system is triggered. Although originating in the bone marrow, mast cells are located throughout the body, especially near blood and lymph vessels, in the brain, intestines, and lungs.
- Myeloblast Cell – A myeloblast cell is a type of immature white blood cell, which, upon maturity, is known as a granulocyte. Developing and remaining in the bone marrow, they contain a large, spherical nucleus, and several nucleoli. Like the mast cell, precursor to the infection-fighting leukocyte, the myeloblast, and its mature granulocyte are also part of the immune response system.
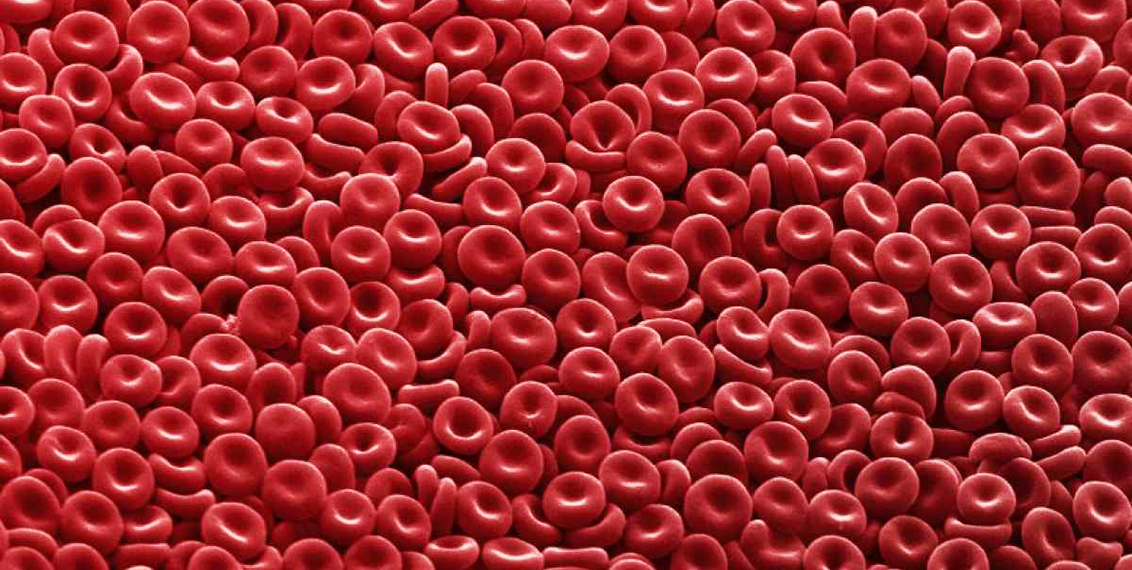
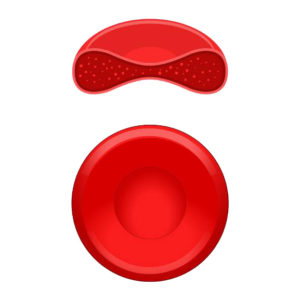 Erythrocyte Cell – Developed in the bone marrow from the hemocytoblast cell, erythrocytes are found throughout the blood and are commonly known as red blood cells (or RBC). Erythrocytes are a crucial component for a healthy functioning body, which contains millions of these round, biconcave cells. Small and flexible, they lack a nucleus, allowing them to move through the thinnest blood vessels. Containing iron-rich hemoglobin, which gives blood its color, their function is to transport oxygen from the lungs to the body’s tissues. On the return trip to the lungs, they carry carbon dioxide, a waste product of metabolism, allowing it to be exhaled. Just one cubic millimeter of blood can contain around 5.5 million erythrocytes, with each living up to four months.
Erythrocyte Cell – Developed in the bone marrow from the hemocytoblast cell, erythrocytes are found throughout the blood and are commonly known as red blood cells (or RBC). Erythrocytes are a crucial component for a healthy functioning body, which contains millions of these round, biconcave cells. Small and flexible, they lack a nucleus, allowing them to move through the thinnest blood vessels. Containing iron-rich hemoglobin, which gives blood its color, their function is to transport oxygen from the lungs to the body’s tissues. On the return trip to the lungs, they carry carbon dioxide, a waste product of metabolism, allowing it to be exhaled. Just one cubic millimeter of blood can contain around 5.5 million erythrocytes, with each living up to four months.
What triggers the process of erythropoiesis?
Erythropoietin, or EPO, is the main hormone responsible for regulating erythropoiesis, ensuring that as erythrocytes die, they are replaced, keeping the ratio equal in a healthy adult. Produced in the liver and kidney when there is a drop in oxygen circulating throughout the body, erythropoietin is a glycoprotein cytokine.
A cytokine is a molecule designed to aid cell to cell communication as part of the immune response system, and a glycoprotein cytokine is a protein with a sugar attached.
Synthetic forms of erythropoietin are used to treat certain medical conditions, increasing the levels of erythrocytes in the body.
What can cause erythropoiesis to become ineffective?
A dysfunction in the production of blood cells can originate from a number of issues, and result in a decrease or increase in activity.
Anemia
This is the most commonly seen disorder with over 6% of the US population affected, and the term covers a whole range of problems. Anemia, or low hemoglobin, is a lack of healthy red blood cells to carry adequate levels of oxygen around the body, and can be the result of decreased production in the bone marrow, or the destruction of red blood cells. The problem can indicate an iron deficiency, possibly due to pregnancy, blood loss or the inability to metabolize iron from the usual nutritional sources.
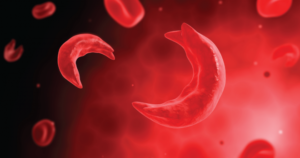
Anemia can also be passed from parent to child. Sickle cell anemia is one such disease and is found mainly in those with an African or Hispanic hereditary background. The normally round blood cells change and become crescent shaped, causing them to form blockages in narrow blood vessels. This results in pain and an inability to deliver oxygen to the organs.
Anemia generally causes the sufferer to feel fatigued and weak, sometimes with feelings of dizziness and an increased heartbeat.
Leukemia
Leukemia is another blood cell disorder. A type of cancer, it mainly affects the over 55 year olds, but in children under 15, it is the most common cancer form. Creating problems with the bone marrow, it results in the production of large numbers of abnormal, underdeveloped blood cells called blasts.
There are several different forms of leukemia, including acute and chronic myeloid leukemia, and acute and chronic lymphoblastic leukemia.
Although the cause of leukemia is still unknown, the medical profession believes there to be both genetic and environmental factors involved. More research is necessary to find the answer to this question.
Kidney disease
 Erythropoietin, the hormone that stimulates the bone marrow to regulate the production of red blood cells, is produced in the kidney. With the presence of kidney disease, erythropoietin amounts lessen, resulting in fewer cells being produced and a diagnosis of anemia being given.
Erythropoietin, the hormone that stimulates the bone marrow to regulate the production of red blood cells, is produced in the kidney. With the presence of kidney disease, erythropoietin amounts lessen, resulting in fewer cells being produced and a diagnosis of anemia being given.
The severity of the anemia is dependent on the amount of damage the kidney has experienced, with the threshold for developing anemia being around one-third of the organ remaining undamaged.
Thalassemia
Thalassemia is an inherited condition that results in decrease of hemoglobin production. Without the hemoglobin to transport the oxygen inside the red blood cells, the body’s organs do not receive the oxygen they need to function effectively.
Thalassemia is seen mainly in those with an Asian, African or Middle Eastern genetic background, and can manifest with little or no symptoms through to its most serious form – Cooley’s anemia, which can be fatal.
Polycythaemia
Polycythaemia, also known as erythrocytosis, is the result of an overproduction of red blood cells. This high concentration can lead to a sluggish blood flow around the body, which can become especially problematic in the smaller, more delicate vessels.
The risk of blood clots means that polycythaemia can become life threatening. Deep vein thrombosis, or pulmonary embolisms can quickly develop as the thickened blood causes blockages, and these, in turn, can lead to strokes or heart attacks.
Erythropoiesis is a crucial process that, in a healthy adult, continues day and night throughout our lives. However, just a small imbalance in the tightly regulated production of erythrocytes, and serious diseases can result. Beginning in the bone marrow, stimulated by erythropoietin from the kidneys, the iron-rich blood cells carry oxygen to all our organs, ensuring the survival of our species.